LIVING WITH THE DAMOCLES SYNDROME
Children with cancer have a much better chance leaves their families with greater uncertainty
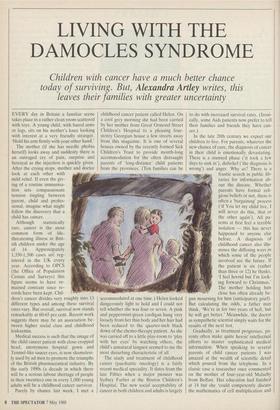
EVERY day in Britain a familiar scene takes place in a rather clean room scattered with toys. A young child, with bared arms or legs, sits on his mother's knee looking with interest at a very friendly stranger. 'Hold his arm firmly with your other hand.'
Medical success is such that the image of the child cancer patient with close-cropped head, anonymous hospital gown and Tenniel-like saucer eyes, is now shameless- ly used by ad men to promote the triumphs of the British pharmaceutical industry. By the early 1990s (a decade in which there will be a serious labour shortage of people in their twenties) one in every 1,000 young adults will be a childhood cancer survivor.
Purely by chance last week, I met a childhood cancer patient called Helen. On a cool grey morning she had been carried by her mother from Great Ormond Street Children's Hospital to a pleasing four- storey Georgian house a few streets away from this magazine. It is one of several houses owned by the recently formed Sick Children's Trust to provide month-long accommodation for the often distraught parents of long-distance' child patients from the provinces. (Ten families can be accommodated at one time.) Helen looked dangerously light to hold and I could not tell whether she was four or seven. A pink and peppermint-green cardigan hung very loosely from her thin body and her hair had been reduced to the quarter-inch black down of the chemo-therapy patient. As she was carried off to a little play-room to 'play with her eyes' by watching others, the child's unnatural languor seemed to me the most disturbing characteristic of all.
The study and treatment of childhood cancer (paediatric oncology) is a fairly recent medical speciality. It dates from the late Fifties when a major pioneer was Sydney Farber at the Boston Children's Hospital. The new social acceptability of cancer in both children and adults is largely to do with increased survival rates. (Ironi- cally, some Aids patients now prefer to tell their families and friends they have can- cer.)
Gradually, as treatment progresses, pa- rents often make quite heroic' intellectual efforts to master sophisticated medical information. When speaking to several parents of child cancer patients I was amazed at the wealth of scientific detail which poured from the telephone. In a classic case a researcher once commented on the mother of four-year-old MalachY from Belfast. Her education had finished at 14 but she 'could competently discuss the mathematics of cell multiplication and
their therapeutic significance in the treat- ment of his acute leukaemia'.
In their distinguished book, The Damo- cles Syndrome (McGraw Hill, 1981), Gerald Koocher and John O'Malley look at new problems peculiar to the first generation of American childhood cancer long-term survivors. They also talk about the efforts made by parents to deal emo- tionally with the 'complex and contradic- tory task' of bringing up a child in 'long- term uncertainty, balancing an awareness of the possibility of death with a realistic hope for cure'. One British mother, whose daughter died of leukaemia in the Sixties recently contrasted her own experience. 'In the Sixties, when cancer treatment was not so advanced, parents knew the out- come and tried to live to the full the time they had left. Now they've got to accept the illness might come back. It must be terrible for parents to live year after year With uncertainty.' The watchfulness a mother had for her child as a newborn baby is now acutely revived for years.
What to tell a child about its illness perplexes many parents. To be as truthful as possible within the terms of its under- standing seems to be the best way. Chil- dren who don't ask questions usually still want to know and other children ask about their illnesses obliquely — 'I suppose I won't get any Christmas presents this Year.' Recently I spoke to a woman whose eight-year-old son, Thomas, came 'off treatment' for a form of cancer of the lymph glands last September. She is secretary of SPoCC (The Society of Pa- rents of Children with Cancer), founded in 1985 and now with 250 member families.
'We've always called Thomas's illness "silly cells". The first time I was washing his hair in the bath [after treatment began] I noticed it coming out in handfuls and this seemed a good time to bring it up. "You know the medicine you have to take to make your silly cells behave themselves? Well, it's going to make your hair come out for a while, but then it will grow back." ' Apart from hair loss (easier for boys because 'even little girls of four are con- scious of their hair') side-effects include vomiting, weight loss because of nausea and 'foot flop'. One drug affects the ankles and the child loses the ability to walk for several days. 'On day eight he used to get a pain above and below one eye that used to make him sob.'
As for other illnesses, young children With cancer are eased into their treatments by the explanatory use of toys and photo- graphs. To give one instance, it is less of a Shock to wake one day in hospital from a 'magic sleep' with a Hickman line stitched in- to your chest, if you have already helped for several days to put a Hickman line into a teddy bear's chest. (This is a special tube for taking blood samples and giving drugs to avoid the constant use of 'needles'.) Modern child cancer patients usually go to school, play normally and go off on excur-
sions ('one child with no hair is an oddity but a coach-load seems normal'). But side-effects can sometimes make going back to school rather unpleasant. 'All his hair had fallen out because of radio- therapy and because of steroids he had the classic "moon-face". When he returned to school after six months, neither the teacher nor the other children in his form recog- nised him.'
Willing a child to live takes a vast amount of emotional energy. When her anxiety is at its height, the mother of a sick child can unintentionally neglect her other children. They too need to understand their brother or sister's illness. ('Why do people buy him presents all the time?') Damaging misunderstandings can occur. When one little girl was untruthfully told that her brother's kidney had been re- moved 'because he had a bad fall', she blamed herself because she had once pushed him over. Sometimes the brothers and sisters of a sick child appear to develop the same symptoms when craving for atten- tion. 'Some worry that if a sibling dies at a certain age, they will also die when they reach that age.'
On top of all this, childhood cancer families often develop severe financial problems. A few days ago, I spoke to a Midlands man whose younger daughter, aged two, was recently found to have a brain tumour. Some months later, the company he was with encouraged him to resign. 'I didn't actually lose a lot of time, but the firm wanted people to give 110 per cent all the time.' The man felt that if he resigned (rather than be sacked) he 'might stand a better chance of getting a job again' after his daughter improved. His wife had already given up a part-time job to look after the child. Families like this are helped by the Malcolm Sargent Cancer Fund for Children (set up by Promenaders in 1968 as a memorial to our late 'ambassador with a baton'). Usually the fund makes discre- tionary grants for travelling to and from distant specialist hospitals, rent arrears and, where necessary, funeral expenses. But now Sylvia Darley of the Malcolm Sargent Fund has discovered that under the new Social Security changes affecting charities, 'if we give families like this more than £250 per year — not a vast sum — they will lose some Social Security be- nefits. Families with a child cancer patient are being penalised.'
The strain of families with a child cancer patient has been also sometimes exacer- bated by the under-funding of the National Health Service. Knowing what the side- effects of their treatment are likely to be, most children get 'psyched-up' for it. But, as an SPoCC parent recently remarked, 'sometimes last year children were turning up for treatment at Birmingham Children's Hospital to be turned away again because there were no beds that day.' Similarly, last year when the Kenton Ward dealing with paediatric oncology was closed at St Barth- olomew's, West Smithfield, child cancer patients were moved into other wards. This may have satisfied some politicians but as one parent pointed out, 'These children have depressed immune systems. Moving them into other wards just means the parents worry more about them getting measles or chickenpox which in these children can be fatal.'
The inadequacies of relying too heavily on charitable fund-raising can be also seen in the area of paediatric oncology. Three years ago to treat brain tumours in children private funds were raised by Bart's to build a radio-isotope room (a special lead-lined treatment room for radio-active patients). The cost was £3/4m. This sum was raised by the hospital itself but steeply rising build- ing costs in central London moved the financial target to £2 million. 'We've now raised £1.5-2 million but the cost has risen again to £3 million. We asked the North- East Thames Regional Health Authority to underwrite the deficit to allow construction work to start but they have just refused.'
Unavoidable 'conflict' between charities is also becoming apparent. In order to modernise Great Ormond Street Chil- dren's Hospital (whose central staircase is actually standing crumbling in scaffolding) the hospital administration has launched the Wishing Well Appeal for £40 million. This is going quite strongly, but one consequence has been to detract attention from smaller charities like the Sick Chil- dren's Trust, desperately trying to increase much-needed parents' accommodation close to the hospital. The need for mothers to he close to children in hospital was re- cognised by the Platt Report as long ago as 1959.
The day when a child goes 'off treat- ment' sometimes warrants a celebration ('we held a party because he'd "made it" '). But as the years pass by without any recurrence of the illness (one, two, five, and on to as many as 17) a new unexpected difficulty can await the childhood cancer survivor as he grows up — discrimination in adult life. Throughout the late Seventies and Eighties, several surveys have been carried out in the United States revealing discrimination against cancer survivors in the fields of employment, life insurance and, of course, health insurance. Adoption agencies were also felt to discriminate against cancer survivors. (Some adults are infertile as a result of cancer treatments given during childhood and when married are likely to apply to become adoptive parents.) People who had struggled va- liantly with disease in childhood and in some cases had been in perfect health for more than 15 years suddenly found them- selves unwanted by employers suspicious of 'absenteeism' and increased insurance premiums.
In Britain, as the new generation of childhood cancer survivors grows up, the need to educate prospective employers is gradually being recognised. At a UKCCSG (United Kingdom Children's Cancer Study Group) conference held on this subject last autumn in Edinburgh, one speaker re- marked that when applying for a job 'a history of cancer is perhaps analagous to or even worse than a criminal record'. Large- ly, it seems to be a question of doctors educating doctors. Medical inspectors in- volved in insurance, employment and adoption are usually still unaware that childhood cancer is no longer a chronic disease and that survivors are normal people. Sitting in his small friendly NHS room (filled with jolly polaroid snapshots of past patients) one paediatric oncologist put it like this: 'It has been light for some hours, but now the sun is coming up.'
The fact that 60-65 per cent of childhood cancer patients now survive also means that 35-40 per cent do not. For these parents, allowing a child to die in the security and normality of home whilst being kept pain-free is the anguishing ideal. It is the cup all parents hope will pass from them. Where funding permits (a bleak fiscal thought) paediatric oncology centres now run small 'symptom care teams' — two or three specially trained medical staff who help parents to make dying children as comfortable as possible. The willingness of the parents gently to acknowledge impending death is also im- portant. There are few things more painful than to see a child dying in tragic isolation because its parents are unable to accept the truth it has already understood.
A few days ago I spoke to a woman whose six-year-old son died at home of leukaemia in August 1985. She has an older daughter and recently gave birth to another son. 'Although he was only six he knew that he was going to die and because it seemed to ease his mind, we did not deny it. I wept every time he asked if I could still come and visit him.' Like other parents whose children die at home, she took him into bed with her during his last months 'to be near him in the night. When I held him in bed as a baby I never thought his life would end like this.' This mother explained that dying is not just 'like switching off a light'. Her son became slowly weaker, there were gradual 'steps downwards' and sometimes lapses into unconsciousness. 'I always thought he would die in the night but eventually he died one August after- noon propped up in a downstairs bed with the family round him as usual.' Among the dimly understood comings and goings of those we love, it was, for this little boy, a moment of peaceful resolution.
Donations would be welcomed by the Sick Children's Trust, 139 Gray's Inn Road, London WCI X 8UB.






















































 Previous page
Previous page